Hundreds of venomous snakes. King Cobras. Spitting cobras. Mambas. Gaboon vipers. African vipers. South American vipers. North American vipers. Every type of snake imaginable. That’s what fascinated Steve Mackessy, Ph.D., from an early age, thanks to his part-time job in high school — working at a reptile supply company. He’s been enthralled with these venomous creatures ever since. Now, he is a professor of Biology in UNC’s College of Natural and Health Sciences.

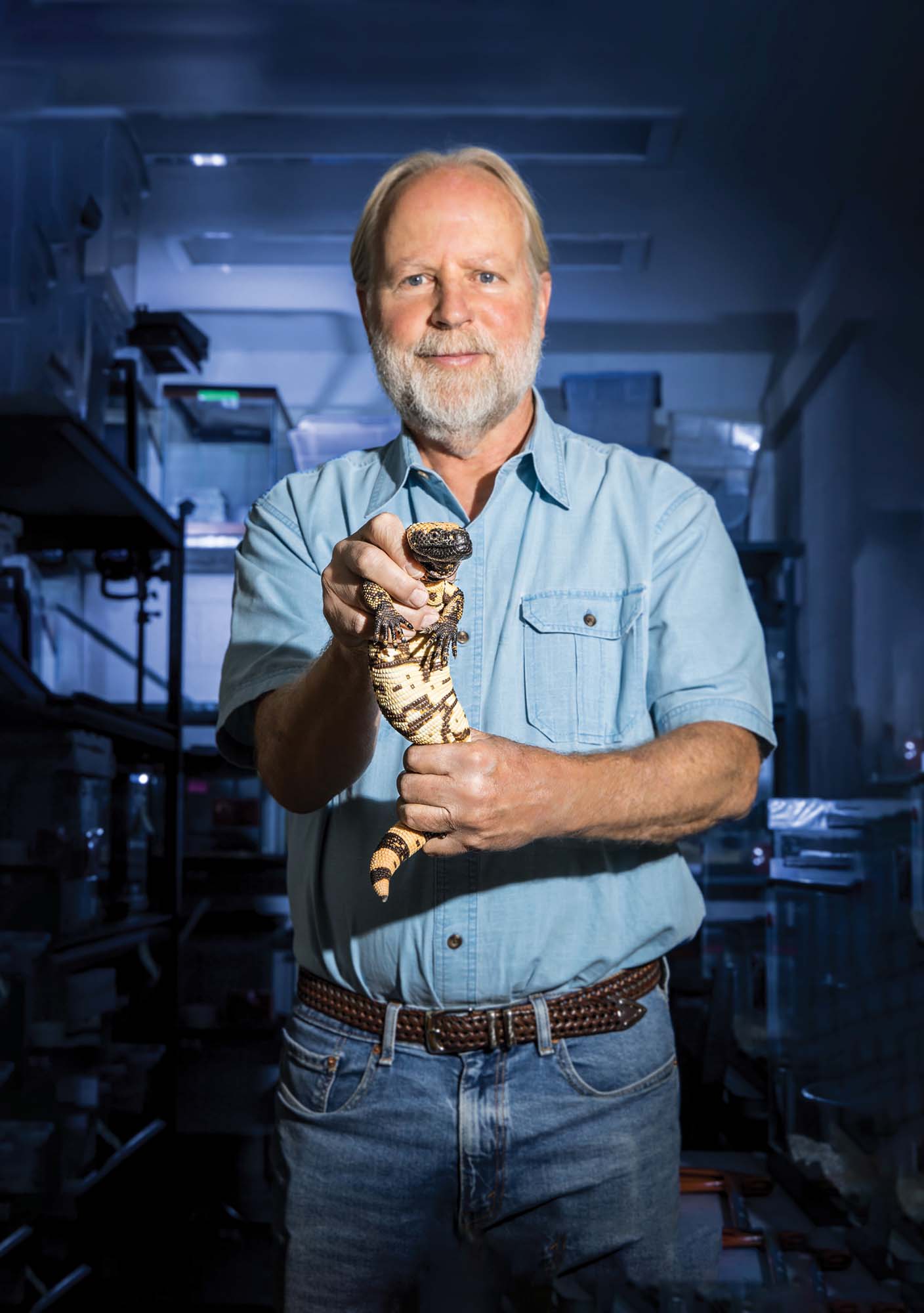
“It is intriguing to me that small animals like venomous snakes and Gila monsters can produce such a myriad of toxins — and how they safely store this bioweapon, what it is biochemically and how purified toxins can be repurposed as therapeutic drugs is even more fascinating!” said Mackessy.
Today, the world-renowned expert in snake venom biochemistry and proteomics runs the Mackessy Venom Analysis Lab (MVAL) at UNC. The lab focuses on identifying the compounds in snake venom that can improve the health of people with debilitating diseases and disorders.
“The general focus of my research is on venomous snakes and their venoms,” explains Mackessy. “However, particular research projects involve very different aspects of the biology of these remarkable animals, ranging from functional biochemistry to population molecular genetics to natural history/ecology.”
From California to Colorado: A Journey in Venom Research
The southern California native earned his bachelor’s and master’s degrees in Evolution/Ecology at the University of California Santa Barbara and his doctorate in Zoology and Biochemistry from Washington State University. He was a postdoctoral research associate in Biochemistry at Colorado State University. Mackessy joined UNC in 1991 as an adjunct instructor and was hired into a tenure-track position in 1994.
Over the past three decades, Mackessy’s lab has been funded by prestigious national and regional grant agencies, including the National Institutes of Health, the National Sciences Foundation, Colorado Parks and Wildlife, the Bureau of Land Management and the Colorado Office of Economic Development and International Trade.
Mackessy has published more than 200 scientific papers, book chapters and natural history notes and several books, garnering more than 9,000 citations. He was the managing editor of the Journal of Natural Toxins for seven years and currently serves on the editorial boards of three journals: Toxins, The Scientific World Journal and Journal of Venom Research.
The Gila Monster: A Deadly Bite
Mackessy’s research gained international attention following the first fatality from a Gila (pronounced “hee-la”) monster bite in 90 years. In February 2024, Christopher Ward, a 34-year-old man from Englewood, Colorado, died after he was bitten by his pet Gila monster. The autopsy revealed that Ward died from complications of what must have been an excruciating, four-minute bite to his right hand.

The Gila monster, a slow-moving reptile that can grow to two feet, is the only venomous lizard native to the United States and one of only two venomous lizards in the world. Though venomous, Gila monsters are retiring animals that bite only when threatened or harassed. Mackessy’s early research focused on Gila monster venom, making him uniquely qualified to investigate this case.
“It was kind of a return to my roots. [The fatality and the focus on Gila monster venom] was one reason we wanted to bring the lizard back here, so we could extract venom and answer some of the questions that we have about it,” Mackessy said.
To investigate why Ward died from a typically non-lethal Gila monster bite, Mackessy teamed up with a colleague, Dr. Nick Brandehoff, a medical toxicologist and reptile expert in the Denver area and a consulting physician in the case. The research team brought the Gila monster to the lab for comparisons between the one that bit Ward and another one obtained years ago from New Mexico.
Their findings were surprising. The basic biochemistry of the two venoms was quite similar, but the Gila monster that bit Ward produced 10 times more venom than the other lizard. “That was one of the very noteworthy things,” Mackessy explained.
“These animals use venom defensively, whereas rattlesnakes and other venomous snakes typically use it offensively. And it’s often based on how they feel.” This proved part of the biologist’s working hypothesis — that this lizard was really agitated, and when they’re agitated, they produce a lot of venom.
The research revealed that Ward likely received an extremely high dose of venom due to the lizard’s agitated state and the prolonged four-minute bite.
“Rattlesnakes strike and release very quickly, and in about a fourth of a second, it’s deposited a large volume of venom,” said Mackessy. “But some Gila monsters hold on for quite a while, which is apparently what this one did.
“Gila monster venom systems are really weird,” Mackessy noted. “Their glands are in the lower jaw, and the teeth that deliver the venom are grooved, so it’s a very inefficient delivery system compared to rattlesnakes.”
It was important to study two similar Gila monsters. “Even with the same species, they have their differences, where they’re from, their age … all that can affect their venom,” said Mackessy. By extracting venom from two Gila monsters, the researchers could compare the results to understand what might have contributed to the man’s rapid decline and eventual death.
From Venom to Medicine: The Science of Drug Discovery
Located on the second floor of Ross Hall, the Mackessy Lab is a vibrant setting for scientific discovery that attracts visiting scholars from around the world. It’s also a wonderland for UNC students drawn to discovering and harnessing venom compounds with promise for drug discovery research and development.
The lab houses many different species of snakes, which are the source of the crude venoms extracted every two months. Many of these venoms are not commercially available from any other sources, making the Mackessy Lab a unique and valuable resource in the field.
Once enough venom is available, researchers work to isolate venom toxins, purify specific components and stabilize them for future testing. This approach allows the researchers to process small amounts of venom rapidly, screen them for potentially useful medicinal compounds and utilize new sequencing methods to determine the primary structure of target molecules in a more cost-effective way. This is a critical early step in the molecular characterization of potential therapeutics.
In collaboration with colleagues, the Mackessy Lab uses innovative techniques like mass spectrometry to analyze venom samples. This approach helps researchers identify and understand proteins in the venom, compare venoms from different species and evaluate venom diversity.
The ultimate goal is to learn more about the biochemistry of venom. Biochemistry and molecular biology have become the foundation for understanding all biological processes and essentially life. This approach to investigating snake venom can lead to identifying novel compounds that could result in new drugs to address debilitating diseases and improve human health.
Circling back to early Gila monster research, in 1990 an endocrinologist in the Bronx studying the venomous lizard’s saliva led to the discovery of the hormone exendin-4, similar to one humans release after eating to control blood sugar levels. The hormone was later synthesized into the drug exenatide used to treat type 2 diabetes.
“There are other peptides in Gila monster venom,” continues Mackessy. “One drug based on these peptides that is being used right now is Ozempic, which was initially designed as another type of drug agonist that stimulates the body to regulate blood sugar glucose.”
Inspired by Gila monster venom, the popular drug Ozempic used to treat diabetes and obesity was brought to market in 2017. The discovery of Ozempic, based on research that began in the 1970s, like most basic science resulted from the work of many scientists, emphasizing that science is iterative, and it could be 20, 30, 40 or 50 years before developing a drug.
“We’re interested in therapeutic drug discovery, and we collaborate with people from all over the world on some of these projects,” said Mackessy. “We can do a lot of the basic science, but taking drugs to market requires additional expertise.” The work that Mackessy and his research team do is anything but basic.
Current Research: Improving Human Health
The Mackessy Lab is currently working on several drug discovery projects, including:
- Purifying specific proteins from rattlesnake venoms.
- Identifying substances with unique effects on blood coagulation or cancer cells.
- Exploring compounds that show potential in limiting metastasis in several types of human cancers.
Evaluating a minibinder protein that could revolutionize snakebite treatment in remote areas.
In a paper published several years ago, Mackessy and his team found that a compound from Russell’s viper venom has the potential to be an effective antithrombotic agent, a promising treatment for clotting disorders that cause strokes. Several substances appear to be effective clot-promoting agents to control bleeding, which has strong emergency medical implications.
Making a Global Impact
Mackessy’s global reputation as a snake expert has resulted in speaking invitations at conferences in Spain, England, India and Brazil, as well as at many conferences and universities in the United States. Mackessy has been the subject of numerous local, national and international news stories, blogs and TV shows, including on the Discovery Channel and BBC.
As a result, the snake venom expert has attracted students to his lab who have continued their work around the world. For example, he hosted visiting Fulbright scholar Dr. Melisa Benard Valle from the Instituto de Biotecnologîa, UNAM in Cuernavaca, Mexico, who visited his lab several times spending three or four months here working with students. She is now a postdoctoral fellow at the Center for Antibody Technologies in Denmark and is currently collaborating with Mackessy on his latest research project involving a minibinder protein. The project has shown encouraging results in mice who receive a minibinder protein after receiving a venom toxin.
“We can actually rescue the mouse, and they survive,” said Mackessy. “Until you show it [can work] in a living system, it’s hard to say you’ve got something that’s actually going to work.”
The breakthrough could have a global impact. In remote parts of the world, there are snakes that produce lethal toxins that kill people very quickly. People in the rural areas of Africa, Asia and South America are most at risk and least able to afford treatment. Currently, people are treated with antibodies from horses, sheep or other large animals but that’s expensive, explains Mackessy, and it’s not available in a lot of places plus it takes a while to get it.
If these minibinder protein molecules prove effective, then scientists may be able to produce injectable shots or oral pills that can be stored easily on a shelf in extremely rural areas.
“If somebody gets bitten by a mamba or cobra or something, you could give them a couple of these tablets with drugs X, Y and Z that target these different toxins in the venom. It may not cure them, but it does keep them from suffering the most severe effects, including death. And gives them more time to get to a clinic,” said Mackessy.
Nurturing the Next Generation of Scientists
A vital part of Mackessy’s work is mentoring students. He has worked with generations of undergraduate and graduate students, many of whom have secured excellent positions in universities, biotech companies and governmental agencies. Several undergraduate students who worked in his lab have become successful physicians, research scientists and scientific professionals in a variety of fields.
“UNC is small, but big enough. The students are very pleasant to work with. They don’t have the attitude of entitlement that we see in some of the bigger schools,” said Mackessy. “Some of our students are absolutely stellar and would be competitive anywhere, Ivy League schools, etc.”
Sam Kerwin, a current Ph.D. student who works in Mackessy’s lab, has conducted several of the onsite analyses of Gila monster venoms. In June, Kerwin and graduate student Eric Januszkiewicz presented at the international scientific symposium Venom Week IX in Durham, North Carolina.
Mackessy has been widely recognized for his work in and out of the classroom, garnering top awards for excellence in research and teaching at UNC.
Former students like Anthony Saviola, Ph.D. ’15, now a research scientist in Biochemistry and Molecular Genetics at the University of Colorado Anschutz, continue to collaborate with Mackessy on groundbreaking research.
Saviola explored the actions of “non-toxic toxins” — known as disintegrins — found only in viper venoms and found that it allows rattlesnakes to relocate prey they bit — simply by scent trail. In later studies, he also found that this same molecule helps to prevent cancer cells from spreading to other parts of the body. This is an excellent example of how the snake uses a molecule in the venom for one purpose — finding its prey — but when purified, scientists can use it for an entirely different purpose, as a potential anti-cancer drug.
“When cancer cells become metastatic and they leave the site of a tumor,” explains Mackessy, “they become dangerous because they can set up tumors throughout the body. This level of penetration into tissues defines the severity, or stages, of the cancer.”
Saviola found these molecules effective in preventing certain cancers from spreading, an idea that was sparked in the Mackessy Lab when he was a graduate student.
“We’re not the first ones or the tenth ones to come up with the idea of using disintegrins [to stop the spread of cancer cells]. A group at USC developed a disintegrin from copperhead snake venom and they took [the research] quite far and started clinical trials,” Mackessy said.
Other alumni, such as Cassandra Modahl, Ph.D. ’16, have gone on to work at prestigious institutions like the Liverpool School of Tropical Medicine and Disease. After completing her Ph.D. in Mackessy’s lab, Modahl obtained a postdoctoral research position in Singapore in one of Mackessy’s colleague’s labs. Currently, she’s working on venom projects at the Liverpool School of Tropical Medicine and Disease, the first institution in the world dedicated to research and teaching tropical medicine.
“I just saw her at a Gordon Research Conference in Maine that I was chairing this summer. She was one of the speakers we invited to talk to about her research. So yeah, that’s cool,” said Mackessy.
Undergraduates at UNC also find their way to Mackessy’s lab as they pursue a chance to make a difference.
“I remember we had a high school dropout who was diagnosed with cancer at age 19, survived that and decided to turn things around and do something different with his life,” said Mackessy. “He initiated cancer cell research in my lab as an undergraduate, and he’s now a practicing physician trained at the Mayo Clinic and has his own practice in Montana.”
As Mackessy continues his pioneering work in venom research, he remains committed to pushing the boundaries of science while inspiring the next generation of researchers. His work at UNC not only contributes to our understanding of venomous creatures but also holds the promise of saving lives through innovative drug discoveries.